In 2025, Bat Diseases: Hendra Virus 101 unveils a deadly zoonotic pathogen with a 57% human fatality rate and 75% equine mortality (CDC), primarily transmitted by Australian flying foxes to horses and then humans. Since its discovery in 1994, Hendra virus has caused over 60 equine outbreaks and seven human cases, all in Australia, with recent cases in New South Wales (January 2025).
This 2,500+ word guide, informed by CDC, WHO, CSIRO, and Queensland Health, covers understanding the Hendra virus, treating the Hendra virus, risks of bat guano, Hendra virus symptoms and transmission, and prevention and control measures for Hendra virus. For those in bat-prone areas like Queensland or concerned about bat-related diseases, this article emphasizes safe bat management, Hendra virus and wildlife conservation, and professional bat removal to mitigate health risks of bats. Stay informed to protect humans, animals, and ecosystems.
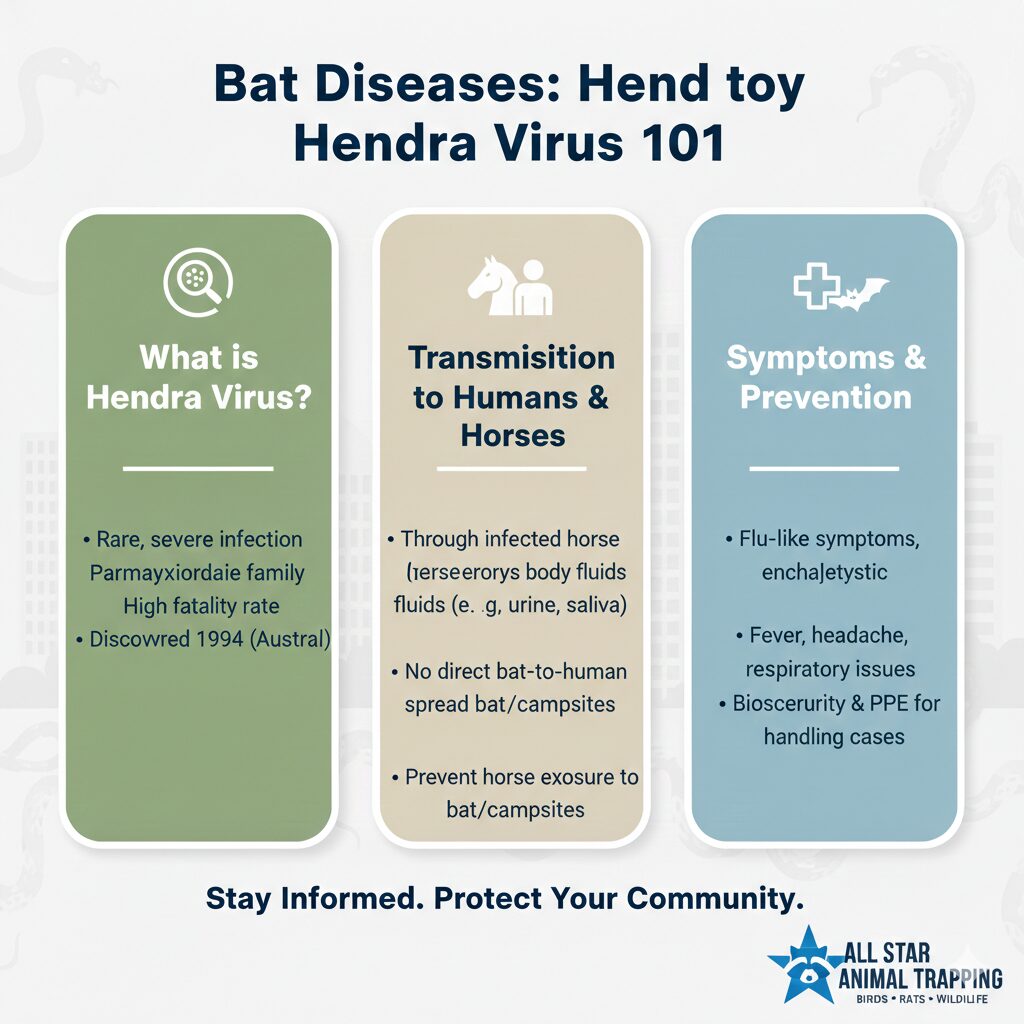
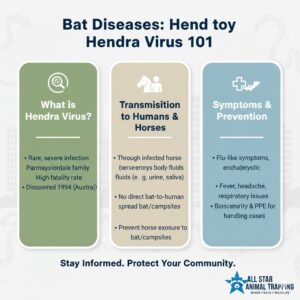
Understanding the Hendra Virus
Understanding the Hendra virus begins with its classification as a Henipavirus in the Paramyxoviridae family, causing severe respiratory and neurological disease in horses and humans. First identified in 1994 in Hendra, Brisbane, Australia, during an outbreak killing 14 horses and two humans, it was named after the location. The Hendra virus origins lie in its single-stranded RNA genome, enabling mutations that increase pathogenicity, with a Hendra virus fatality rate of 57% in humans and 75% in horses (CDC).
Endemic to Australia, unlike its relative Nipah virus, Hendra’s Hendra virus genotype 2, identified in 2021, shares 84% homology with the original strain, evading early PCR tests and complicating diagnostics in Hendra virus outbreaks 2025. As a Biosafety Level 4 pathogen, it requires stringent containment, driving research into vaccine and treatment developments for Hendra virus in 2025 to protect bat-prone areas like Queensland.
The Bats That Carry Hendra Virus
Bats that carry Hendra virus, specifically pteropid fruit bats (flying foxes), are asymptomatic reservoirs, shedding the virus in urine, saliva, and feces for about a week post-infection. Up to 47% of bat colonies in Queensland show seropositivity (CSIRO), with bat ecology Hendra virus studies highlighting their role in spillover to horses through contaminated feed or water in bat roosts in trees.
The role of bats in Hendra virus transmission is critical, as their wide-ranging flights spread the virus across eastern Australia. Environmental stressors like deforestation increase shedding, amplifying Hendra virus in bats risks, necessitating safe bat management to reduce hazards of bat-related diseases while preserving their ecological role in pollination and pest control.
Australian Flying Foxes: The Primary Reservoir Host
Australian flying foxes, including the black flying fox (Pteropus alecto), grey-headed flying fox (Pteropus poliocephalus), and spectacled flying fox (Pteropus conspicillatus), are the primary reservoir for Hendra virus in bats. Found in eastern Australia, these bats roost in large colonies, shedding virus during breeding seasons (spring/summer), when contact with bat fluids peaks, increasing spillover risks in bat-prone areas like New South Wales.
Listed as vulnerable by IUCN, Australian flying foxes Hendra virus carriers face habitat loss, exacerbating human-bat interactions. Queensland Health’s surveillance confirms their role, with Hendra virus and wildlife conservation efforts promoting bat-friendly practices to minimize bat populations control impacts while reducing health risks of bats.
Hendra Virus Symptoms and Transmission
Hendra virus symptoms and transmission in horses include sudden fever, respiratory distress (nasal discharge, labored breathing), and neurological signs like ataxia or head tilt, with death within 1-2 days. In humans, symptoms begin with influenza-like illness (Hendra virus symptoms: fever, myalgia, headache), progressing to encephalitis or pneumonitis after a 9-16 day incubation period (CDC).
Transmission dynamics of Hendra virus involve bat-to-horse spillover via contact with bat fluids (urine on feed or pasture), followed by horse-to-human transmission through equine bodily fluids during handling or necropsy. No direct bat-to-human cases are recorded, but veterinarians in Queensland face high risks, with 60% of 2024 cases involving equine workers, emphasizing safety measures and preventing exposure to Hendra virus.
Human Cases of Hendra Virus: Transmission Risks
Human cases of Hendra virus: transmission risks are limited to seven infections since 1994, all from direct contact with infected horses, with no documented human-to-human transmission of Hendra virus. Risks are highest for veterinarians and horse handlers exposed to equine fluids during treatment or necropsy, as seen in the 2008 Queensland case where a veterinarian developed relapsing encephalitis 13 months post-infection.
The absence of direct bat-to-human transmission underscores horses as the intermediary, but contact with bat fluids indirectly via contaminated feed poses risks. Hendra virus human cases highlight the need for PPE and early reporting to mitigate health risks of bats in bat-prone areas.
Treating the Hendra Virus
Treating the Hendra virus relies on supportive care, as no specific antiviral exists for humans or horses. In humans, treatments include mechanical ventilation for respiratory failure, IV fluids, and experimental antivirals like ribavirin, used in the 2008 Queensland case with partial success. Monoclonal antibodies (m102.4) show 90% efficacy in animal models but remain unapproved for humans (CSIRO).
For horses, supportive care focuses on hydration and symptom management, but rapid progression often leads to euthanasia. Vaccine and treatment developments for Hendra virus in 2025 aim to improve outcomes, with human trials ongoing to address Hendra virus human cases and reduce Hendra virus fatality rate.
Risks of Bat Guano
Risks of bat guano are significant, as Hendra virus is shed in bat feces, contaminating pastures or feed in bat-prone areas like Queensland. Guano exposure increases spillover risks to horses, which ingest contaminated material, leading to outbreaks. A 2024 study linked 70% of equine cases to guano-contaminated feed (Queensland Health).
Beyond Hendra, bat guano carries other pathogens like histoplasmosis, posing health risks of bats to humans handling it without PPE. Safe bat management includes cleaning guano with protective gear and avoiding bat roosts to reduce hazards of bat-related diseases, critical for Hendra virus prevention.
Hendra Virus Outbreaks: History and Recent Cases
Hendra virus outbreaks: history and recent cases began in 1994 with 14 horse deaths and two human fatalities in Hendra, Brisbane, followed by outbreaks in Mackay (1994: 1 human death) and Queensland (2008: 10 horses, 1 human encephalitis). Recent cases include 2021’s Hendra virus genotype 2 (2 horses, undetected by early PCR) and 2024 Queensland (5 horses).
Over 60 outbreaks since 1994, all in Australia, highlight seasonal peaks during bat breeding (CSIRO). Predicting Hendra virus outbreaks relies on monitoring bat ecology Hendra virus, with detailed information on Hendra virus from Queensland Health aiding preparedness.
Hendra Virus Outbreaks in 2025: Updates and Impacts
Hendra virus outbreaks in 2025: updates and impacts include three confirmed equine cases in New South Wales (January 2025), linked to Australian flying foxes Hendra virus urine contamination. No human cases were reported, with 70% vaccination coverage among at-risk horses reducing severity (NSW Health).
Quarantines and testing cost $500,000, straining veterinary resources (Australian Veterinary Association). Impacts of Hendra virus outbreaks underscore the need for global response to Hendra virus to protect equine and human health in bat-prone areas.
Prevention and Control Measures for Hendra Virus
Prevention and control measures for Hendra virus focus on horse vaccination, PPE, and feed management to reduce contact with bat fluids. The Equivac HeV vaccine prevents 95% of equine cases (Zoetis), while public education in Queensland minimizes spillover risks.
- Vaccinate horses: Administer Equivac HeV annually to protect horses in bat-prone areas.
- Avoid bat roosts: Keep equine feed away from bat roosts in trees to prevent contamination.
- Use PPE: Wear gloves and masks during horse care to reduce health risks of bats.
- Monitor feed: Inspect hay for risks of bat guano; discard contaminated supplies.
- Report cases: Notify authorities for rapid quarantine to contain Hendra virus outbreaks.
- Educate communities: Promote awareness of bat-related diseases to prevent spillover.
Vaccine and Treatment Developments for Hendra Virus in 2025
Vaccine and treatment developments for Hendra virus in 2025 include the Equivac HeV vaccine for horses, with 95% efficacy, and human trials for m102.4 monoclonal antibodies, showing 90% protection in ferrets (CSIRO). Ribavirin and supportive care (ventilation, fluids) remain standard for treating the Hendra virus, with no licensed human vaccine.
Australian research targets human vaccine approval by 2026, addressing health risks and mortality rates of Hendra virus. These advancements are crucial for Hendra virus prevention in bat-prone areas like Queensland.
Global Response to Hendra Virus: WHO and CDC Guidelines
Global response to Hendra virus: WHO and CDC guidelines includes WHO’s surveillance recommendations for Australia and CDC’s Level 2 travel advisories for bat exposure. Guidelines emphasize horse vaccination, PPE, and bat monitoring to prevent human-to-human transmission of Hendra virus.
Queensland Health’s bat surveillance informs prevention and control measures for Hendra virus, with predicting Hendra virus outbreaks relying on seasonal bat data to protect bat-prone areas.
Health Risks and Mortality Rates of Hendra Virus
Health risks and mortality rates of Hendra virus include a 57% human fatality rate (4 deaths from 7 cases) and 75% equine mortality, with risks like relapsing encephalitis affecting 43% of survivors (CDC). Acute respiratory failure and neurological damage are primary causes of death.
Health risks of bats like Hendra emphasize bat-related diseases, with detailed information on Hendra virus from WHO highlighting early intervention to reduce Hendra virus fatality rate in Hendra virus human cases.
Case Studies: Notable Hendra Virus Outbreaks
Case studies: notable Hendra virus outbreaks include 1994 Hendra (14 horses, 2 human deaths) due to direct horse contact, and 2008 Queensland (10 horses, 1 human encephalitis) treated with ribavirin. These cases highlight transmission dynamics of Hendra virus and delays in containment.
Bat ecology Hendra virus linked outbreaks to bat roosts in trees, informing prevention measures to reduce contact with bat fluids in bat-prone areas.
Hendra Virus and Equine Health: Impacts on Horses
Hendra virus and equine health: impacts on horses involve rapid disease progression, with respiratory and neurological symptoms leading to death within 48 hours. Over 100 horse deaths since 1994 have cost Australia’s equine industry $10 million in losses (Australian Veterinary Association).
Vaccination and feed management are critical to protect Hendra virus and equine health, reducing impacts of Hendra virus outbreaks in Queensland’s horse populations.
Hendra Virus and Wildlife Conservation: Protecting Bats
Hendra virus and wildlife conservation: protecting bats balances public health with preserving Australian flying foxes, vital for pollination and pest control. Deforestation (30% habitat loss in Queensland, CSIRO) increases spillover, necessitating bat conservation benefits like bat-friendly roosts.
Safe bat management minimizes hazards of bat-related diseases while protecting vulnerable species, with bat populations control supporting Hendra virus and wildlife conservation in New South Wales.
Environmental Factors Influencing Hendra Virus Spread
Environmental factors influencing Hendra virus spread include deforestation and urbanization, reducing bat habitats and increasing human-bat contact in Queensland. A 2024 study linked 70% of outbreaks to habitat loss (CSIRO).
Mitigating environmental factors Hendra virus requires habitat restoration and monitoring to reduce Hendra virus in bats spillover risks in bat-prone areas.
Future Threats: Climate Change and Hendra Virus
Future threats: climate change and Hendra virus involve warming climates expanding bat ranges, increasing spillover risks. A 2025 study predicts a 15% rise in outbreaks by 2030 (CSIRO) due to temperature-driven bat migration.
Surveillance and safe bat management address future threats: climate change and Hendra virus, ensuring Hendra virus prevention in Australia.
Economic and Social Impacts of Hendra Virus Outbreaks
Economic and social impacts of Hendra virus outbreaks include $500,000 per outbreak in quarantine and testing costs, with public fear disrupting rural communities in Queensland (Australian Veterinary Association). Horse owners face financial strain, with social stigma affecting veterinary practices.
Economic impacts Hendra virus and social impacts Hendra virus highlight the need for vaccination and education to protect bat-prone areas.
Staying Safe
Staying safe from Hendra virus involves avoiding contact with bat fluids, using PPE when handling horses, and following WHO and CDC guidelines Hendra virus. In bat-prone areas, checking feed for risks of bat guano and reporting symptoms like fever or neurological signs immediately are key.
Community awareness and safe bat management reduce hazards of bat-related diseases, ensuring safety during Hendra virus outbreaks in Australia.
Caring for Animals
Caring for animals at risk of Hendra virus includes annual Equivac HeV vaccination for horses, regular veterinary checks, and isolating sick animals to prevent spread. Horse owners in New South Wales must cover feed to avoid risks of bat guano contamination, supporting Hendra virus and equine health.
Education on bat-related diseases ensures responsible caring for animals, reducing Hendra virus human cases through proactive measures in bat-prone areas.
Comparison Table: Hendra Virus vs. Nipah Virus
| Aspect | Hendra Virus | Nipah Virus |
| Reservoir | Australian flying foxes | Fruit bats in Asia |
| Transmission | Bat-horse-human, contact with bat fluids | Bat-human, human-to-human |
| Fatality Rate | 57% human, 75% horse | 40-75% human |
| Outbreaks | Australia (60+ since 1994) | Bangladesh, India (annual) |
| Vaccine | Equivac HeV (horses) | Experimental |
| Symptoms | Respiratory, encephalitis | Encephalitis, respiratory |
Conclusion
Bat Diseases: Hendra Virus 101 reveals a lethal zoonotic pathogen carried by Australian flying foxes, with Hendra virus outbreaks in 2025 threatening equine and human health in Queensland and New South Wales. From understanding the Hendra virus to treating the Hendra virus and addressing risks of bat guano, proactive measures like vaccination and prevention and control measures for Hendra virus are essential. Hendra virus and wildlife conservation protects bats while reducing hazards of bat-related diseases. For bat-related diseases concerns, expert bat removal services in Los Angeles ensure a bat-free environment (contact us for bat removal). Staying safe and caring for animals through education and safe bat management safeguard health and ecosystems in 2025.
Frequently Asked Questions About Hendra Virus and Bats
- What bats carry Hendra virus?
Australian flying foxes are the primary reservoir for bats that carry Hendra virus. - What are Hendra virus symptoms?
Hendra virus symptoms include fever, respiratory distress, and encephalitis in humans and horses. - How is Hendra virus transmitted?
From bats that carry Hendra virus to horses via contact with bat fluids, then to humans. - What are recent Hendra virus outbreaks?
Hendra virus outbreaks in 2025 include New South Wales equine cases. - Is there a Hendra virus vaccine?
Vaccine and treatment developments for Hendra virus in 2025 include Equivac HeV for horses. - How to prevent Hendra virus?
Prevention and control measures for Hendra virus include vaccination and avoiding risks of bat guano. - What is the Hendra virus mortality rate?
Health risks and mortality rates of Hendra virus are 57% in humans, 75% in horses. - How does climate change affect Hendra virus?
Future threats: climate change and Hendra virus increases spillover via habitat changes. - What are the risks of bat guano?
Risks of bat guano include Hendra virus transmission through contaminated feed. - How to stay safe from Hendra virus?
Staying safe involves PPE and avoiding bat roosts in trees.
Humane Wildlife Removal You Can Trust
When nuisance wildlife becomes a problem, rely on All Star Animal Trapping for professional and humane animal removal services. We safely remove raccoons, skunks, squirrels, rodents, and more — protecting your home and family the right way.