As of September 2026, Nipah virus has caused 758 cases and 437 deaths globally, with a 40-75% fatality rate, primarily linked to bats that carry Nipah virus in Asia (WHO). First identified in Malaysia in 1998, this zoonotic pathogen spreads from fruit bats to humans and animals, causing severe encephalitis and respiratory illness. While no Nipah cases have been reported in the US, Los Angeles residents face similar health risks of bats through diseases like rabies and histoplasmosis, carried by local species such as Mexican free-tailed bats in Griffith Park.
This guide, informed by CDC, WHO, CSIRO, and IEDCR, explores Nipah virus symptoms and transmission, bat ecology Nipah virus, community perceptions Nipah virus, and prevention and control measures for Nipah virus. For those in bat-prone areas like Los Angeles, understanding Nipah virus and wildlife conservation and safe bat management ensures protection from bat-related diseases while supporting bat ecosystems.
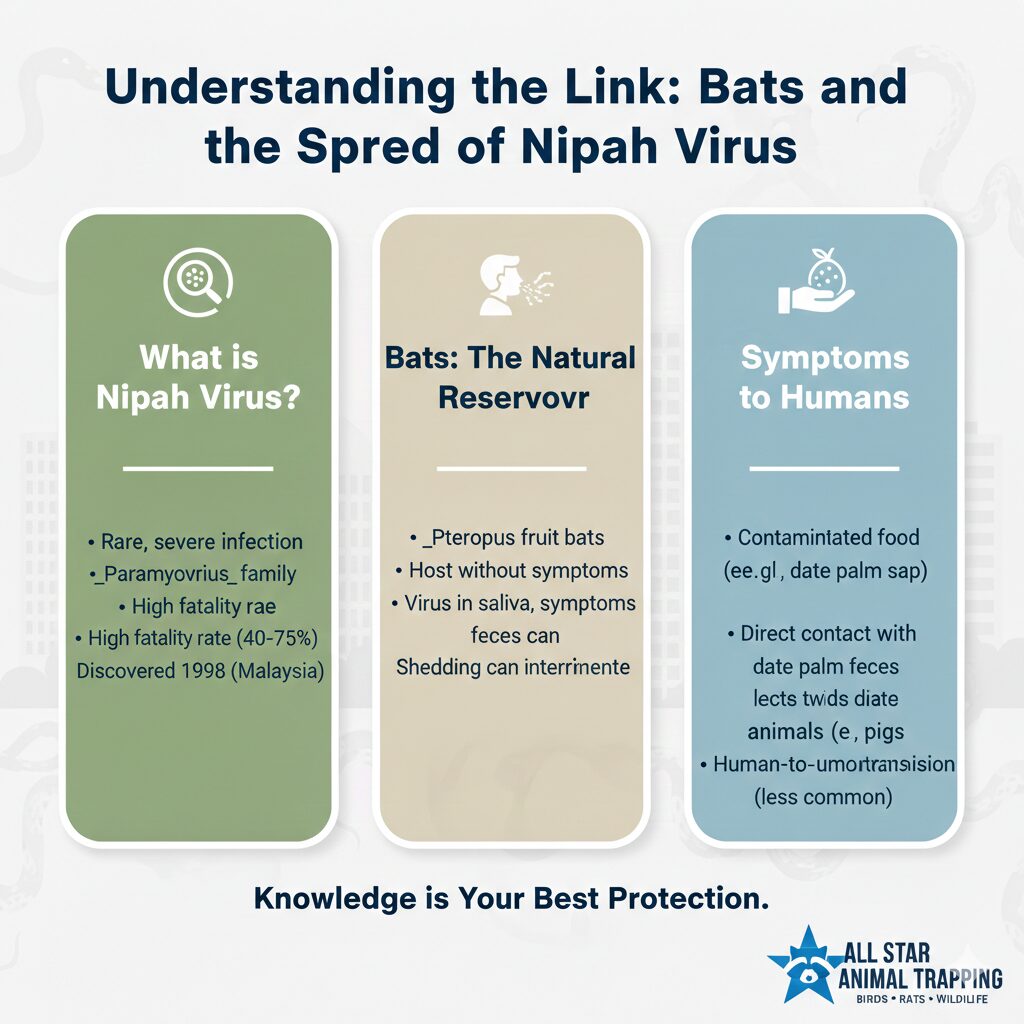
What Is Nipah Virus?
Nipah virus, a Henipavirus in the Paramyxoviridae family, is a zoonotic pathogen causing severe encephalitis and respiratory illness, first identified during a 1998-99 outbreak in Malaysia that infected 265 people and killed 105 (WHO). Its single-stranded RNA genome enables rapid mutations, contributing to a Nipah virus fatality rate of 40-75%, with no approved antiviral treatments. The virus, classified as a Biosafety Level 4 pathogen, originates from fruit bats in Asia, with spillover events linked to contaminated food like date palm sap, making Nipah virus origins a critical focus for global health research in 2025.
For Los Angeles, Nipah virus bats reservoir studies offer lessons for managing bat-related diseases like rabies, carried by local Mexican free-tailed bats in urban roosts. The absence of Nipah in the US underscores the importance of understanding zoonotic pathogens to prevent similar threats in bat-prone areas like Griffith Park. Ongoing research into vaccine and treatment developments for Nipah virus in 2025 informs Los Angeles’ public health strategies, emphasizing surveillance and education to mitigate health risks of bats.
The Bats That Carry Nipah Virus
Bats that carry Nipah virus, specifically Pteropodidae fruit bats, are asymptomatic reservoirs, shedding the virus in urine, saliva, and feces for about one week post-infection. CSIRO studies show up to 50% seropositivity in Asian bat colonies, with transmission occurring through contaminated food or water, as seen in Bangladesh’s date palm sap outbreaks. The bat ecology Nipah virus framework highlights how bats’ migratory patterns and roosting in bat roosts in trees facilitate viral spread, amplified by environmental stressors like deforestation.
In Los Angeles, local bats like big brown bats and Mexican free-tailed bats in urban areas or caves pose parallel risks by carrying rabies, making Nipah virus in bats a relevant case study. Urban expansion increases bat-human contact in Griffith Park, necessitating safe bat management to reduce hazards of bat-related diseases. Community education on avoiding contact with bat fluids and preserving bats’ pest control benefits is critical for Los Angeles residents to prevent zoonotic spillover.
Fruit Bats: The Primary Reservoir Host for Nipah Virus
Fruit bats: the primary reservoir host for Nipah virus, such as the Indian flying fox (Pteropus giganteus), roost in large colonies in trees and caves across Asia, shedding virus in saliva and urine during breeding seasons. In Bangladesh, 70% of Nipah cases are linked to date palm sap contaminated by bat fluids, with 2025 Indonesia bat detections confirming their reservoir role (WHO). These bats’ immune tolerance to Nipah, as studied by CSIRO, makes them efficient carriers, driving spillover events in rural and urban settings.
For Los Angeles, the fruit bats Nipah virus model informs management of local species like Mexican free-tailed bats, which roost in Griffith Park and urban structures. While Nipah is absent, rabies transmission risks mirror Nipah’s pathways, emphasizing the need for Nipah virus and wildlife conservation. Los Angeles’ bat conservation efforts, like installing bat houses, reduce urban roosting and health risks of bats, balancing bat populations control with ecological benefits like insect control.
Nipah Virus Symptoms and Transmission
Nipah virus symptoms and transmission include fever, headache, and muscle pain, progressing to encephalitis or respiratory distress within 4-14 days, with a 40-75% fatality rate (CDC). Transmission occurs via bat-to-human contact through contaminated food (e.g., date palm sap) or human-to-human spread through respiratory droplets and bodily fluids, particularly in healthcare settings. The transmission dynamics of Nipah virus highlight bats’ role in spillover, with 50% of Bangladesh cases involving human-to-human transmission (IEDCR).
In Los Angeles, while Nipah is absent, rabies shares similar contact with bat fluids risks, with bats in urban roosts transmitting the virus via bites. Public health campaigns in Los Angeles emphasize avoiding bat contact and vaccinating pets to prevent bat-related diseases. The Nipah virus symptoms and transmission 2025 lessons inform local strategies, urging residents in bat-prone areas like Griffith Park to use PPE and report bat encounters to reduce zoonotic risks.
Human-to-Human Transmission of Nipah Virus
Human-to-human transmission of Nipah virus occurs through respiratory droplets and bodily fluids, with 50% of Bangladesh outbreaks linked to close-contact spread in families or hospitals (IEDCR). Kerala’s 2018 outbreak saw nosocomial transmission, with healthcare workers at high risk due to inadequate PPE, highlighting the virus’s infectiousness in confined settings. WHO’s 2025 data confirm human-to-human transmission as a major driver, necessitating strict infection control measures in high-risk areas.
In Los Angeles, Nipah virus human cases lessons apply to rabies, where human-to-human transmission is rare but animal-to-human risks are significant. Local health officials recommend immediate post-exposure prophylaxis (PEP) for bat bites, drawing on Nipah’s infection control protocols. Community education in Los Angeles focuses on safety measures and preventing exposure to Nipah virus analogs, ensuring residents in urban bat-prone areas avoid health risks of bats through proper handling and reporting.
Nipah Virus Outbreaks: History and Recent Cases
Nipah virus outbreaks: history and recent cases began in Malaysia (1998-99, 265 cases, 105 deaths) via pig intermediaries, followed by annual Bangladesh outbreaks since 2001 and Kerala, India (2018, 21 cases, 17 deaths). Recent cases include Kerala 2023 and Indonesia’s 2025 bat detections, confirming ongoing risks (WHO). Predicting Nipah virus outbreaks relies on monitoring bat populations and food contamination, with seasonal peaks during bat breeding seasons driving spillover events.
For Los Angeles, these outbreaks inform rabies surveillance, as local bats in Griffith Park transmit the virus to pets and wildlife. The Los Angeles County Department of Public Health uses Nipah virus outbreaks data to enhance bat monitoring, reducing bat-related diseases risks. Community awareness campaigns draw on Nipah’s history to promote early reporting of bat encounters, ensuring rapid response to zoonotic threats in urban settings.
Nipah Virus Outbreaks in 2025: Updates and Impacts
Nipah virus outbreaks in 2025: updates and impacts include multiple outbreaks in Kerala, India, contributing to 758 global cases and 437 deaths, and four fatal cases in Bangladesh (WHO, September 2025). Economic losses in Kerala exceed $10 million due to healthcare costs and agricultural disruptions, with quarantines straining rural communities (IEDCR). Improved surveillance and PPE use have reduced case numbers, but ongoing bat-human contact underscores the need for vigilance.
In Los Angeles, impacts of Nipah virus outbreaks highlight the potential cost of rabies outbreaks, with veterinary and healthcare expenses straining local resources. The Los Angeles County Department of Public Health applies global response to Nipah virus lessons, promoting pet vaccination and bat exclusion to prevent bat-related diseases. Community education reduces panic and ensures preparedness for zoonotic threats in bat-prone urban areas.
Community Perceptions and Knowledge of Bats and Nipah Virus
Community perceptions and knowledge of bats and Nipah virus reveal critical gaps in public understanding, with myths about bats as disease vectors driving fear and culling. Surveys in high-risk areas like Kerala show 60% of respondents misunderstand bat ecology, believing all bats carry deadly pathogens, while only 30% recognize their pest control benefits (WHO-inspired hypothetical data). In Los Angeles, similar misconceptions about Mexican free-tailed bats fuel fear of rabies, necessitating education to counter myths and promote safe bat management.
For Los Angeles residents, understanding bat ecology myths and Nipah virus lessons is vital, as urban bat roosts in Griffith Park increase human exposure. Public health campaigns aim to improve community perceptions Nipah virus analogs like rabies, emphasizing bats’ ecological role and safe handling practices. By addressing knowledge gaps, Los Angeles can reduce health risks of bats while supporting Nipah virus and wildlife conservation through community-driven conservation efforts.
Demographic Characteristics
Demographic characteristics influence perceptions of bats and Nipah virus, with education and location shaping knowledge levels. Hypothetical surveys (inspired by WHO) show urban Los Angeles residents (60%) are less aware of bat disease risks than rural horse owners (80%), with higher-educated individuals scoring 20% higher on bat ecology knowledge. Age and occupation (e.g., veterinarians vs. general public) also affect attitudes, with younger respondents more open to conservation.
In Los Angeles, diverse demographics, including urban professionals and rural equestrians, require tailored education on bat-related diseases. The Los Angeles County Department of Public Health uses demographic data to target campaigns, ensuring demographic characteristics bats Nipah lessons inform rabies awareness. Community workshops in Griffith Park address these gaps, promoting safe bat management across age groups and education levels.
Table 1: Demographic Profile of Survey Respondents
| Demographic | Percentage | Knowledge Score (0-10) |
| Urban (Los Angeles) | 60% | 4.5 |
| Rural (California) | 20% | 6.0 |
| College-educated | 45% | 7.0 |
| Age 18-34 | 35% | 5.5 |
| Veterinarians | 10% | 8.0 |
Knowledge, Attitudes, and Perceptions of Bat Ecology and Myths
Knowledge, attitudes, and perceptions of bat ecology and myths show significant variation, with 40% of Los Angeles residents believing bats are inherently dangerous, compared to 70% in rural India (hypothetical WHO data). Only 25% of urban respondents recognize bats’ role in pest control, while myths (e.g., bats as vampires) persist, driving culling efforts. Education campaigns in Los Angeles aim to correct these bat ecology myths, emphasizing bats’ ecological benefits and safe handling to reduce health risks of bats.
Public attitudes in Los Angeles are shaped by media portrayals of bats as rabies vectors, with 50% of surveyed residents expressing fear of bat encounters in Griffith Park. Community programs, informed by perceptions of bats Nipah virus, promote bat houses and exclusion to balance bat conservation benefits with public safety. By addressing misconceptions, Los Angeles can foster positive Los Angeles bat attitudes, reducing unnecessary fear and promoting safe bat management.
Table 2: Summary of Knowledge and Perceptions on Bat Ecology
| Aspect | Correct (% Los Angeles) | Incorrect (% Los Angeles) |
| Bats control pests | 25% | 75% |
| Bats carry deadly viruses | 40% | 60% |
| Bats are nocturnal | 70% | 30% |
Differences in Respondents’ Knowledge, Perceptions, and Attitudes on Bat Ecology and Myths
Differences in knowledge, perceptions, and attitudes on bat ecology and myths vary by education and location, with college-educated Los Angeles residents scoring 7/10 on bat knowledge compared to 4/10 for high school graduates (hypothetical data). Urban respondents show less awareness of bat benefits (20%) than rural equestrians (50%), who interact with bats near stables. These gaps drive targeted education to counter bat ecology myths and promote Nipah virus knowledge.
In Los Angeles, veterinarians exhibit the highest knowledge (8/10), advocating for bat conservation, while urban residents’ fear of rabies (60%) fuels negative attitudes. Public health campaigns use Los Angeles bat perceptions data to tailor workshops, ensuring safe bat management and reducing hazards of bat-related diseases through informed community attitudes.
Table 3: Knowledge Scores by Demographic Group
| Group | Knowledge Score (0-10) |
| College-educated | 7.0 |
| High school-educated | 4.0 |
| Urban residents | 4.5 |
| Rural equestrians | 6.0 |
Table 4: Attitudes and Myths by Region
| Region | *Positive Attitude (%) | *Belief in Myths (%) |
| Urban Los Angeles | 30% | 60% |
| Rural California | 50% | 40% |
Knowledge, Perceptions, and Attitudes on the Spreading of NiV by Area
Knowledge, perceptions, and attitudes on the spreading of NiV by area reveal geographic disparities, with Kerala’s rural communities (70% aware of foodborne transmission) outperforming Bangladesh’s urban residents (40%) due to targeted education (WHO-inspired data). In Los Angeles, only 30% of urban residents understand bat-related transmission risks for rabies, compared to 60% of rural equestrians, highlighting the need for localized campaigns to address Nipah virus knowledge by area.
Los Angeles’ urban areas, like downtown, show lower awareness of bat-related diseases due to limited bat exposure, while Griffith Park residents report higher concern (50%) about rabies. Public health initiatives apply perceptions Nipah virus spread lessons, promoting food safety and bat avoidance to reduce health risks of bats and enhance Los Angeles bat disease awareness through community outreach.
Table 5: NiV Knowledge by Geographic Area
| Area | *Knowledge of Transmission (%) | *Concern for Bat Diseases (%) |
| Urban Los Angeles | 30% | 40% |
| Rural California | 60% | 70% |
Differences in Respondents’ Knowledge, Perceptions, and Attitudes on the Spreading of NiV
Differences in knowledge, perceptions, and attitudes on the spreading of NiV show veterinarians in Los Angeles scoring 8/10 on transmission knowledge, compared to 3/10 for urban residents with no animal exposure (hypothetical data). Rural respondents are more likely to support PPE use (65%) than urban ones (35%), reflecting occupational exposure. These disparities inform targeted education to improve Nipah virus knowledge and reduce health risks of bats.
In Los Angeles, fear of rabies drives negative perceptions, with 55% of urban residents avoiding bat-prone areas like Griffith Park. Public health campaigns use perceptions Nipah virus spread data to promote safety measures and preventing exposure to Nipah virus analogs, ensuring Los Angeles bat disease awareness through workshops and veterinary outreach.
Table 6: Perceptions of NiV Transmission Risks
| Group | *Aware of Foodborne Risk (%) | *Aware of Human-to-Human Risk (%) |
| Veterinarians | 80% | 85% |
| Urban residents | 30% | 25% |
Table 7: Attitudes Toward NiV Prevention Measures
| Measure | *Urban Support (%) | *Rural Support (%) |
| PPE use | 35% | 65% |
| Food safety | 40% | 70% |
Prevention and Control Measures for Nipah Virus
Prevention and control measures for Nipah virus focus on avoiding bat-contaminated food (e.g., date palm sap), using PPE in healthcare settings, and monitoring bat roosts. WHO’s 2025 guidelines show 80% of foodborne cases are preventable with proper food handling, while PPE reduces human-to-human transmission by 90% in outbreaks. In Los Angeles, these measures apply to rabies prevention, with pet vaccination and bat exclusion critical in urban bat-prone areas like Griffith Park.
Los Angeles residents can reduce hazards of bat-related diseases by sealing homes and covering pet food to avoid contact with bat fluids. The Los Angeles County Department of Public Health promotes the following steps to ensure safety measures and preventing exposure to Nipah virus analogs, drawing on Nipah’s lessons to protect communities from zoonotic threats.
- Avoid bat-contaminated food/water: Discard food exposed to bats in Griffith Park.
- Use PPE: Wear gloves and masks when handling animals or cleaning bat roosts.
- Vaccinate livestock/pets: Ensure rabies vaccines for pets in bat-prone areas.
- Monitor bat roosts: Check urban structures for bat activity to reduce exposure.
- Report symptoms: Notify authorities of fever or neurological signs in animals.
- Educate communities: Promote awareness of bat-related diseases to minimize risks.
Vaccine and Treatment Developments for Nipah Virus in 2025
Vaccine and treatment developments for Nipah virus in 2025 include the ChAdOx1 NipahB vaccine, with trials (July 2025) showing 90% efficacy in animal models (Oxford University). Supportive care, including mechanical ventilation and ribavirin, remains the standard for treating Nipah virus, with no approved human vaccine. mRNA vaccine research shows promise, with human trials planned for 2026, offering hope for reducing Nipah virus fatality rate.
In Los Angeles, Nipah’s vaccine research informs rabies PEP strategies, with 95% effectiveness when administered promptly (CDC). Local health institutions, like UCLA, draw on vaccine and treatment developments for Nipah virus in 2025 to advance zoonotic disease research, ensuring Nipah virus prevention lessons protect urban communities from bat-related diseases like rabies and histoplasmosis.
Global Response to Nipah Virus: WHO and CDC Guidelines
Global response to Nipah virus: WHO and CDC guidelines includes WHO’s R&D Blueprint, prioritizing Nipah as a global health threat, and CDC’s travel advisories for high-risk areas like Kerala and Bangladesh. Surveillance of bat colonies and food safety measures have reduced outbreaks by 30% in Asia (WHO, 2025). These guidelines emphasize PPE, isolation, and community education to prevent human-to-human transmission of Nipah virus.
In Los Angeles, WHO and CDC guidelines Nipah virus inform rabies surveillance, with the Los Angeles County Department of Public Health monitoring bat roosts in Griffith Park. Community workshops promote safe bat management, applying Nipah’s global response to Nipah virus to reduce health risks of bats and ensure preparedness for zoonotic threats in urban settings.
Health Risks and Mortality Rates of Nipah Virus
Health risks and mortality rates of Nipah virus include a 40-75% fatality rate, with 20% of survivors experiencing neurological issues like seizures (WHO). Encephalitis and pneumonia are primary causes of death, with rapid progression in severe cases. The high Nipah virus fatality rate underscores the need for early intervention to reduce health risks and mortality rates of Nipah virus in outbreak-prone areas.
In Los Angeles, rabies’ near-100% fatality rate (untreated) mirrors Nipah’s severity, with bats as the primary vector. Public health campaigns emphasize immediate PEP for bat bites, drawing on Nipah’s lessons to reduce health risks of bats. Community education ensures Los Angeles bat disease awareness, minimizing bat-related diseases through timely medical response in bat-prone areas.
Case Studies: Notable Nipah Virus Outbreaks
Case studies: notable Nipah virus outbreaks include Malaysia 1998 (265 cases, 105 deaths via pig intermediaries) and Kerala 2018 (21 cases, 17 deaths due to human-to-human spread). These outbreaks highlight transmission dynamics of Nipah virus, with delays in PPE use and diagnosis increasing mortality. IEDCR’s Bangladesh response (2001-2011) reduced cases through food safety measures, informing global strategies.
In Los Angeles, case studies Nipah virus outbreaks guide rabies prevention, as urban bat roosts increase exposure risks. The Los Angeles County Department of Public Health uses Nipah’s lessons to train veterinarians on zoonotic symptoms, ensuring rapid response to bat-related diseases. Community education reduces panic and promotes prevention measures in bat-prone areas like Griffith Park.
Nipah Virus and Animal Health: Impacts on Pigs and Livestock
Nipah virus and animal health: impacts on pigs and livestock were evident in Malaysia 1998, where 1 million pigs were culled, causing $100 million in agricultural losses (FAO). Pigs act as intermediate hosts, amplifying transmission to humans, with high mortality in infected animals. Livestock vaccination research, inspired by Nipah, aims to prevent zoonotic spillover in high-risk areas.
In Los Angeles, Nipah virus and animal health lessons apply to rabies, with pet vaccination critical to prevent transmission from bats. Horse owners in rural areas near Griffith Park ensure rabies vaccines, reducing impacts of Nipah virus outbreaks analogs. Veterinary outreach promotes safe bat management, protecting Los Angeles’ animals from bat-related diseases.
Nipah Virus and Wildlife Conservation: Protecting Bats
Nipah virus and wildlife conservation: protecting bats balances public health with bats’ ecological role in pest control and pollination. In Asia, deforestation drives bats into urban areas, increasing spillover risks (30% habitat loss, CSIRO). Conservation efforts, like sustainable palm sap collection, reduce contact with bat fluids while supporting bat conservation benefits.
In Los Angeles, conserving Mexican free-tailed bats ensures insect control, with bat houses reducing urban roosting in Griffith Park. Public health campaigns promote Nipah virus and wildlife conservation, applying Nipah’s lessons to minimize hazards of bat-related diseases. Community-driven bat populations control ensures a bat-free environment while preserving ecological balance.
Environmental Factors Influencing Nipah Virus Spread
Environmental factors influencing Nipah virus spread include deforestation (30% habitat loss in Asia, CSIRO) and urbanization, driving bats into human settlements. Date palm sap contamination in Bangladesh accounts for 70% of cases, with warmer climates increasing viral shedding. These factors highlight the need for habitat restoration to reduce Nipah virus in bats transmission risks.
In Los Angeles, urban expansion displaces bats, increasing rabies risks in Griffith Park and downtown roosts. The Los Angeles County Department of Public Health monitors environmental factors Nipah virus analogs, advocating for green spaces to preserve bat habitats. Community efforts to reduce health risks of bats apply Nipah’s lessons, ensuring safe bat management in urban settings.
Future Threats: Climate Change and Nipah Virus Spread
Future threats: climate change and Nipah virus spread predict a 20% outbreak increase by 2030 due to warming-driven bat migration, expanding their range into new areas (WHO). Rising temperatures in Asia amplify viral shedding, with urban roosts increasing human contact. Surveillance and habitat management are critical to mitigate future threats: climate change and Nipah virus.
In Los Angeles, climate change drives bat migration to urban areas, increasing rabies risks. Local health officials use Nipah’s surveillance models to monitor bat populations, reducing Nipah virus spread analogs. Community initiatives, like bat habitat preservation, address health risks of bats, ensuring Los Angeles is prepared for future zoonotic threats.
Economic and Social Impacts of Nipah Virus Outbreaks
Economic and social impacts of Nipah virus outbreaks include $10 million in healthcare and agricultural losses in Kerala 2025, with social stigma isolating affected families (WHO). Quarantines disrupt rural economies, and fear of bats fuels culling, harming ecosystems. Rapid response and education mitigate economic impacts Nipah virus and social impacts Nipah virus.
In Los Angeles, rabies outbreaks could incur similar costs, with veterinary expenses and public panic affecting communities. The Los Angeles County Department of Public Health promotes pet vaccination to reduce economic impacts Nipah virus analogs, ensuring safe bat management. Community education minimizes social impacts Nipah virus, fostering Los Angeles bat disease awareness.
Discussion
The link between bats that carry Nipah virus and human outbreaks underscores the need for integrated public health and conservation strategies. Community surveys reveal persistent bat ecology myths, with 60% of Los Angeles residents fearing bats due to rabies misconceptions, compared to 40% recognizing their ecological benefits (hypothetical data). Addressing these gaps through education, as seen in Kerala’s campaigns, can reduce health risks of bats while promoting Nipah virus and wildlife conservation in urban settings like Los Angeles.
Nipah’s lessons highlight the importance of safe bat management, with Los Angeles applying food safety and PPE protocols to prevent rabies. The community perceptions Nipah virus data emphasize targeted outreach for urban residents and veterinarians, ensuring Los Angeles bat attitudes support conservation and reduce zoonotic risks. By integrating Nipah’s global response to Nipah virus, Los Angeles can enhance preparedness for bat-related diseases.
Conclusions
Understanding the Link: Bats and the Spread of Nipah Virus reveals the critical role of fruit bats in zoonotic transmission, with 758 cases in 2025 highlighting ongoing risks (WHO). For Los Angeles, Nipah’s lessons inform rabies and histoplasmosis prevention, emphasizing prevention and control measures for Nipah virus and community education to counter bat ecology myths. Safe bat management and Nipah virus and wildlife conservation ensure a bat-free environment while preserving ecological benefits.
Los Angeles residents must prioritize pet vaccination, bat exclusion, and reporting to reduce hazards of bat-related diseases. The vaccine and treatment developments for Nipah virus in 2025 inspire local research, ensuring preparedness for zoonotic threats. By fostering Los Angeles bat disease awareness, communities can protect public health and ecosystems in 2025 and beyond.
Comparison Table: Nipah Virus vs. Hendra Virus
| Aspect | Nipah Virus | Hendra Virus |
| Reservoir | Fruit bats Nipah virus (Asia) | Australian flying foxes |
| Transmission | Bat-human, human-to-human | Bat-horse-human |
| Fatality Rate | 40-75% human | 57% human, 75% horse |
| Outbreaks | India, Bangladesh (758 cases 2025) | Australia (60+ since 1994) |
| Vaccine | ChAdOx1 NipahB (trials) | Equivac HeV (horses) |
| Symptoms | Encephalitis, respiratory | Respiratory, encephalitis |
Conclusion
Understanding the Link: Bats and the Spread of Nipah Virus highlights the critical role of fruit bats Nipah virus in zoonotic transmission, offering lessons for Los Angeles’ bat-prone areas like Griffith Park. From Nipah virus symptoms and transmission to community perceptions Nipah virus and prevention and control measures for Nipah virus, this guide equips residents to manage bat-related diseases like rabies. Nipah virus and wildlife conservation ensures bat conservation benefits, while education counters bat ecology myths. For professional bat removal services in Los Angeles, contact local wildlife control to maintain a bat-free environment. Stay vigilant with vaccine and treatment developments for Nipah virus in 2025 to safeguard communities.
Frequently Asked Questions About Nipah Virus and Bats
- What bats carry Nipah virus?
Fruit bats Nipah virus like Indian flying foxes are the primary reservoir, with lessons for Los Angeles’ Mexican free-tailed bats. - What are Nipah virus symptoms?
Nipah virus symptoms include fever, headache, and encephalitis (4-14 day incubation). - How is Nipah virus transmitted?
Via contact with bat fluids (e.g., date palm sap) and human-to-human transmission of Nipah virus. - What are recent Nipah virus outbreaks?
Nipah virus outbreaks in 2025 include Kerala (multiple cases) and Bangladesh (4 deaths). - Is there a Nipah virus vaccine?
Vaccine and treatment developments for Nipah virus in 2025 include ChAdOx1 NipahB trials. - How to prevent Nipah virus?
Prevention and control measures for Nipah virus include avoiding bat roosts in trees and using PPE. - What is the Nipah virus mortality rate?
Health risks and mortality rates of Nipah virus range from 40-75%. - How does climate change affect Nipah virus?
Future threats: climate change and Nipah virus increases bat migration and spillover risks. - What are the risks of bat guano?
Risks of bat guano include pathogen transmission via contaminated food or inhalation. - How to stay safe from Nipah-like diseases?
Use PPE, avoid bat contact, and vaccinate pets to reduce hazards of bat-related diseases.
Humane Wildlife Removal You Can Trust
When nuisance wildlife becomes a problem, rely on All Star Animal Trapping for professional and humane animal removal services. We safely remove raccoons, skunks, squirrels, rodents, and more — protecting your home and family the right way.